By Dr Julia Adams (Osteopath) |
Have you ever experienced pain?
I’m guessing the answer is YES. Some people only experience pain infrequently, like when they stub their toe on something and immediately jump back, wincing. For others, pain is a constant, unrelenting, frustration that has a really huge impact on their life.
In the last few years, a lot of new research has been presented about pain, especially chronic, or ongoing, pain. As an Osteopath, understanding pain and addressing the relevant factors that influence it go a long way toward helping patients feel better.
What is pain?
The International Association for the Study of Pain (IASP) defines pain as an unpleasant sensory and emotional experience associated with actual or potential tissue damage. Note the careful wording here – ‘actual or potential tissue damage’. This tells us that it’s not even necessary to experience tissue damage to feel pain, which brings me to an important point
Pain ⇏ damage
Pain can exist completely independently of any damage to your body. Essentially, the mechanism behind pain starts when noxious stimuli (a.k.a. signals from parts of your body) travel via the spinal cord to the brain. It’s then up to the brain to decide whether this message should be perceived as pain.
The main purpose of this mechanism, evolutionarily speaking, is to aid in our survival. If the brain decides that there is a potential threat for tissue damage, pain is a strong signal to alter our behaviour, thus protecting us from damage or preventing further damage. Without this important control mechanism in our brain, humans would continuously do things that cause tissue damage, like burning ourselves or walking on broken bones, which are not helpful for our survival.
Many factors contribute to whether our brain decides if a signal will be registered as pain or not. These include:
- past experiences
- our beliefs, knowledge and culture around pain
- motor patterns.
Source: https://www.painaustralia.org.au/about-pain/what-is-pain
How do children experience pain?
As young children, external cues help us determine what is pain. The way adults respond to children in pain plays a crucial role in a child’s experiences and beliefs about pain.
You might have noticed that sometimes when a toddler trips over, they initially pause, looking to others for acknowledgement that they have experienced pain. If adults respond with gasps and immediately rush over to help the child, they will often start crying. Conversely, if the adults respond calmly, encouraging the child to get up and continue their task, the child will often not even perceive the experience as painful.
From a young age, we learn how to respond to pain. The relationship with pain that we develop as a young child shapes our thoughts and emotions towards pain as we grow into adults.
Why does some pain go away while other pain persists?
Have you ever had pain that lingers around longer than expected? It can become a little worrying and you might start wondering if something is seriously wrong. Why is it not getting better? Am I going to feel this pain for the rest of my life?’
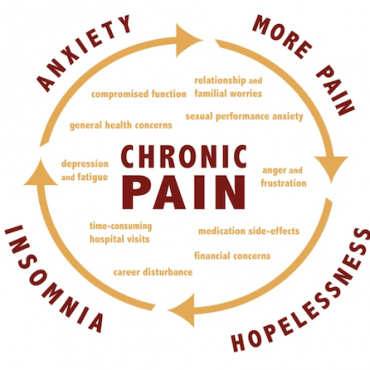
We refer to a new incidence of pain as acute pain. When it starts to linger longer than the expected tissue healing time, or an acute episode returns, we refer to it as chronic pain. As clinicians, we must consider what factors allow acute pain to persist, and develop into chronic pain. It’s important to remember that chronic pain can be a significant financial and mental burden on a patient and their family.
Recent research into chronic pain has provided some important insights. We now know that chronic pain can be associated with structural, functional and biochemical changes in the central nervous system. Significant relationships between traumatic events in childhood and chronic pain have also been identified.
Other factors that increase the likelihood of developing chronic pain include:
- psychosocial deprivation
- past difficulty coping
- substance abuse
- depression
- lack of social support.
As Osteopaths, we try to address some of these factors (when within our scope). In addition to other musculoskeletal findings, addressing these factors can make a big difference in helping the patient deal with chronic pain. We use a wide range of biopsychosocial knowledge to identify when a referral to another practitioner, such as a psychologist or GP, might be more helpful in addressing the factors that are influencing pain.
Resources to help manage pain
When treating chronic pain patients, I often suggest the following educational resources. Research has shown that understanding what pain is, why it occurs, and what can be done about it can positively influence a patient’s outcome.
Books
Pain Heroes is a wonderful, inexpensive book written by Victorian based Osteopath Alison Sim. It is a great read for anyone who has experienced, or is experiencing chronic pain. It includes stories of hope and recovery. You can purchase the book in hardcopy or PDF directly from the Beyond Mechanical Pain website.
Explain Pain by David Butler & Lorimer Moseley (hardcopy)
Recovery Strategies Workbook by Greg Lehman is a free downloadable e-book and awesome resource for practitioners and clients. Highly educational with plenty of practical ideas for managing pain and strategies to get you back to the things you love.
Videos
Understanding Pain in less than 5 minutes (YouTube)
Lorimer Moseley – Why Things Hurt – TEDxAdelaide (YouTube)
Load vs Capacity and Injuries (YouTube)
- Helps explain why some injuries happen.
Want to know more? There is a wealth of knowledge at Melbourne Osteopathy Sports Injury Centre to help increase your understanding of pain. If you’d like to discuss pain, or any other issue, you can contact us at any time:
- (03) 9939 1289
- [email protected]
- Book a consultation online